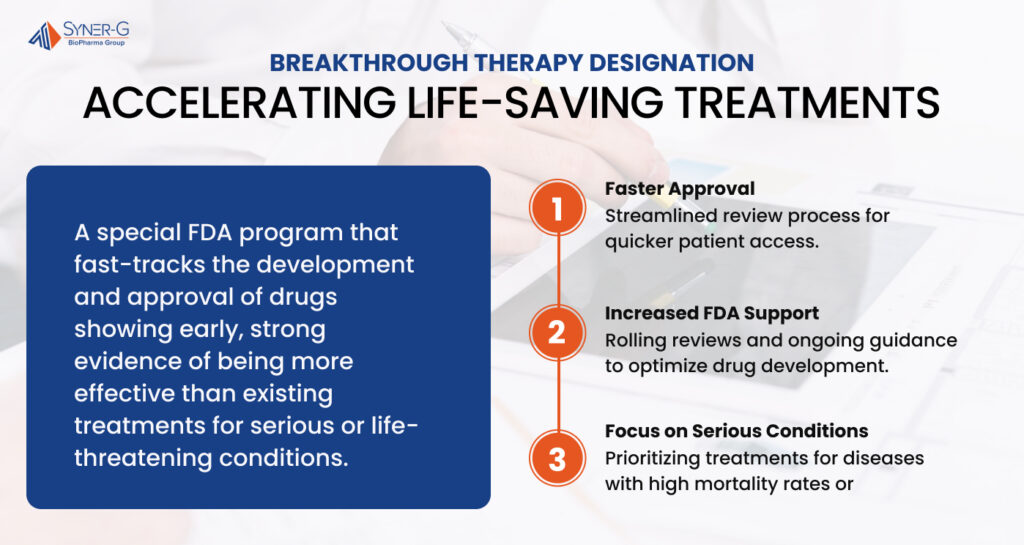
Patients with serious or life-threatening conditions often face limited treatment options, and waiting for new therapies can take years. The Breakthrough Therapy Designation (BTD) helps accelerate this process for drugs that show strong early evidence of being more effective than existing treatments.
With a faster review timeline and increased FDA support, this designation plays a vital role in bringing innovative therapies to those who need them most.
Understanding Breakthrough Therapy Designation
Breakthrough Therapy Designation (BTD) is an FDA program designed to accelerate the development and review of drugs that show early promise in treating serious or life-threatening conditions. Unlike standard drug approvals, this designation aims to help patients gain faster access to therapies that offer a substantial improvement over existing treatments.
To qualify, a drug candidate must meet two key FDA breakthrough therapy designation criteria:
- It must treat a serious condition: This includes diseases with high mortality rates, debilitating symptoms, or conditions that severely impact a patient’s quality of life, such as small cell lung cancer or breast cancer.
- Preliminary clinical evidence must indicate a significant benefit: Early clinical trials must demonstrate that the drug provides a clinically significant improvement over available therapies. This could mean better survival rates, fewer side effects, or enhanced effectiveness in patients who have previously been treated with limited success.
The FDA review process for BTD is designed to streamline drug development timelines. When a drug is granted breakthrough status, the sponsor receives intensive guidance from the FDA to optimize the clinical development process. This includes rolling review, meaning data can be submitted as it becomes available, rather than waiting for a full new drug application (NDA) or biologics license application (BLA) submission.
How Breakthrough Therapy Designation Differs from Other Expedited Programs
The FDA offers multiple expedited approval pathways to speed up access to innovative medicines, but Breakthrough Therapy Designation is distinct from other programs like Priority Review and Fast Track. Here’s how they compare:
- Fast Track: Focuses on drugs that address unmet medical needs, allowing for early and frequent communication with the FDA. However, Fast Track doesn’t necessarily require preliminary clinical evidence of a substantial improvement—it can be granted based on biological plausibility alone.
- Priority Review: Shortens the FDA approval timelines by reducing the standard review period from 10 months to six. Unlike Breakthrough Therapy Designation, Priority Review does not provide early-stage regulatory support or development guidance.
In contrast, Breakthrough Therapy Designation provides the most comprehensive level of FDA support, combining elements of both Fast Track and Priority Review while offering a more hands-on approach to accelerate drug development.
Since the program’s inception, BTD has played a critical role in bringing forward oncology products, antibody-drug conjugates, and other innovative medicines that have transformed treatment options for patients with limited existing therapies. It is one of the most effective tools in enabling patients with serious conditions to access new, life-saving treatments as quickly as possible.

How Does a Drug Qualify for Breakthrough Therapy Designation?
The Breakthrough Therapy Designation (BTD) is reserved for drugs that show strong early clinical evidence of providing a substantial improvement over existing therapies for serious or life-threatening diseases. The FDA breakthrough therapy criteria ensure that only treatments with real potential for transforming patient care receive this accelerated status.
But what does it take for a drug to qualify?
Clinically Significant Endpoints and Addressing Unmet Medical Needs
For a drug to be considered for breakthrough designation, it must meet two essential requirements.
First, early clinical evidence must demonstrate a clear advantage over available therapies. This means the drug must show clinically significant endpoints—such as improved survival rates, reduced disease progression, or superior symptom management—compared to existing treatment options. Unlike traditional approval processes, which often require years of data, preliminary clinical evidence must already suggest that the drug could fundamentally improve patient outcomes.
The second requirement is that the drug must address an unmet medical need. This is especially critical in diseases where existing therapies are limited or ineffective, such as small-cell lung cancer and breast cancer. Many patients in these populations have been previously treated with little success, and breakthrough designation applications prioritize drugs that could demonstrate substantial improvement over existing options.
The FDA Review Process and Expedited Timelines
Once a drug meets these criteria, the FDA review process moves significantly faster than a standard drug application.
Breakthrough therapy status provides sponsors with intensive FDA guidance throughout the clinical development process, ensuring that trial designs are optimized to accelerate data collection and approval.
One of the most significant advantages of BTD is a rolling review, which allows companies to submit parts of their new drug application (NDA) or biologics license application (BLA) as data becomes available, rather than waiting for the full submission. This can shave years off development timelines, giving patients earlier access to promising treatments.
The expedited process also means these drugs may qualify for priority review, further accelerating the approval process.
Breakthrough Therapies That Have Transformed Medicine
Since the program’s inception, multiple BTD drugs have revolutionized treatment landscapes, particularly in oncology products. The New England Journal of Medicine has reported on antibody-drug conjugates that have significantly advanced cancer research, offering targeted therapies for patients who previously had few options. One notable case involved a drug for lung cancer, where preliminary evidence showed a substantial improvement over existing therapies, leading to rapid FDA approval.
These successes highlight why the FDA breakthrough therapy designation is more than just a regulatory shortcut. It is a vital tool in modern medicine, ensuring that treatments backed by strong clinical benefits and early clinical evidence can reach the patients who need them most.

The Role of Breakthrough Therapy Designation in Drug Development
Breakthrough therapy designation accelerates the drug development process for serious or life-threatening conditions by reducing approval timelines and increasing FDA guidance. This designation streamlines the process, ensuring promising treatments reach patients faster than traditional pathways allow.
A major advantage of breakthrough status is a rolling review, which allows sponsors to submit sections of a new drug application or biologics license application as data becomes available. This can significantly shorten development timelines, especially in oncology. Many drugs granted this designation serve previously treated patients who have exhausted existing options, making early access critical.
While the process is faster, clinical trials remain essential. Preliminary clinical evidence must demonstrate substantial improvement over available therapies, with endpoints such as tumor reduction, increased survival rates, or fewer side effects. Strong early data in biologics and antibody drug conjugates has led to priority review and faster approvals, particularly in cancer research.
Since the program’s inception, breakthrough therapy designation has helped bring innovative treatments to market at an unprecedented pace. Case studies in the New England Journal of Medicine highlight how these drugs have changed treatment landscapes, particularly in oncology and rare diseases.
Breakthrough Therapy Designation and Patient Access
Breakthrough therapy designation plays a crucial role in getting life-saving treatments to patients faster. Expediting the drug development process guarantees that those facing serious or life-threatening conditions gain access to promising new therapies sooner than through traditional approval pathways.
The streamlined FDA review process, which includes rolling review and priority review, allows for faster regulatory decisions while maintaining rigorous safety and efficacy standards.
Advocacy organizations like Friends of Cancer Research have been instrumental in pushing for policies that accelerate drug administration safety assessments. Their work has helped shape the regulatory framework that allows breakthrough therapies to move through clinical development more efficiently while making sure that safety data remains a priority. This has been especially critical in oncology, where faster access to effective treatments can make a significant difference in survival rates and quality of life.
For patients who have already undergone multiple treatments with limited success, breakthrough designation offers hope. Many of these drugs are intended for previously treated patients with few existing options.
By addressing unmet medical needs and demonstrating substantial improvement over available therapies, these treatments provide new possibilities for those who might otherwise have no viable alternatives. In cases such as small-cell lung cancer and certain aggressive breast cancers, breakthrough therapies have changed the standard of care, offering extended survival and better outcomes.
Driving Medical Innovation and Expanding Patient Access
Breakthrough therapy designation has reshaped the way innovative treatments reach patients, offering a faster and more efficient pathway for life-saving drugs. By combining expedited timelines with rigorous clinical evaluation, this program allows therapies to demonstrate substantial improvement over existing options and can address urgent medical needs. Its impact is particularly evident in oncology and rare diseases, where early access to breakthrough therapies can mean the difference between life and death.
As the FDA continues to refine and enhance this process, the future of drug development will be driven by speed, innovation, and a commitment to improving patient outcomes.

