Clinical study reports represent the backbone of regulatory submissions in pharmaceutical development. These documents capture the full scope of clinical trial data and analysis, providing regulatory authorities with the evidence needed for approval decisions.
The importance of well-prepared clinical study reports cannot be overstated. Regulatory agencies rely on these documents to understand not just what happened during a trial, but why certain decisions were made and how results should be interpreted. This makes the quality of clinical study report preparation critical for successful regulatory submissions.
What is a Clinical Study Report?
The clinical study report documents every aspect of a clinical trial’s execution and results. Unlike interim reports or study protocols, this comprehensive document presents final outcomes, safety profiles, and statistical analyses that regulators examine during their evaluation process. Each report must demonstrate adherence to good clinical practice guidelines while presenting clear evidence of a drug’s risk-benefit profile.
Modern regulatory requirements have evolved to emphasize clinical study data transparency. Regulatory agencies now expect detailed documentation that allows independent assessment of trial methodology and conclusions. The medical device industry and pharmaceutical sectors both rely on these reports to support marketing applications and post-market surveillance activities.
Study sponsors bear ultimate responsibility for ensuring reports meet regulatory standards. However, the actual document preparation typically involves collaboration between medical writers, biostatisticians, and clinical research teams. This multidisciplinary approach helps address the complex analytical and regulatory requirements that characterize contemporary clinical research.
The content of clinical study reports varies depending on the therapeutic indication and patient population studied. Trials investigating life-threatening diseases require more extensive safety documentation compared to studies in less critical therapeutic areas. Regulatory authorities adjust their review intensity based on these risk considerations.
Related Article: Understanding the Nuances of a Clinical Study Protocol
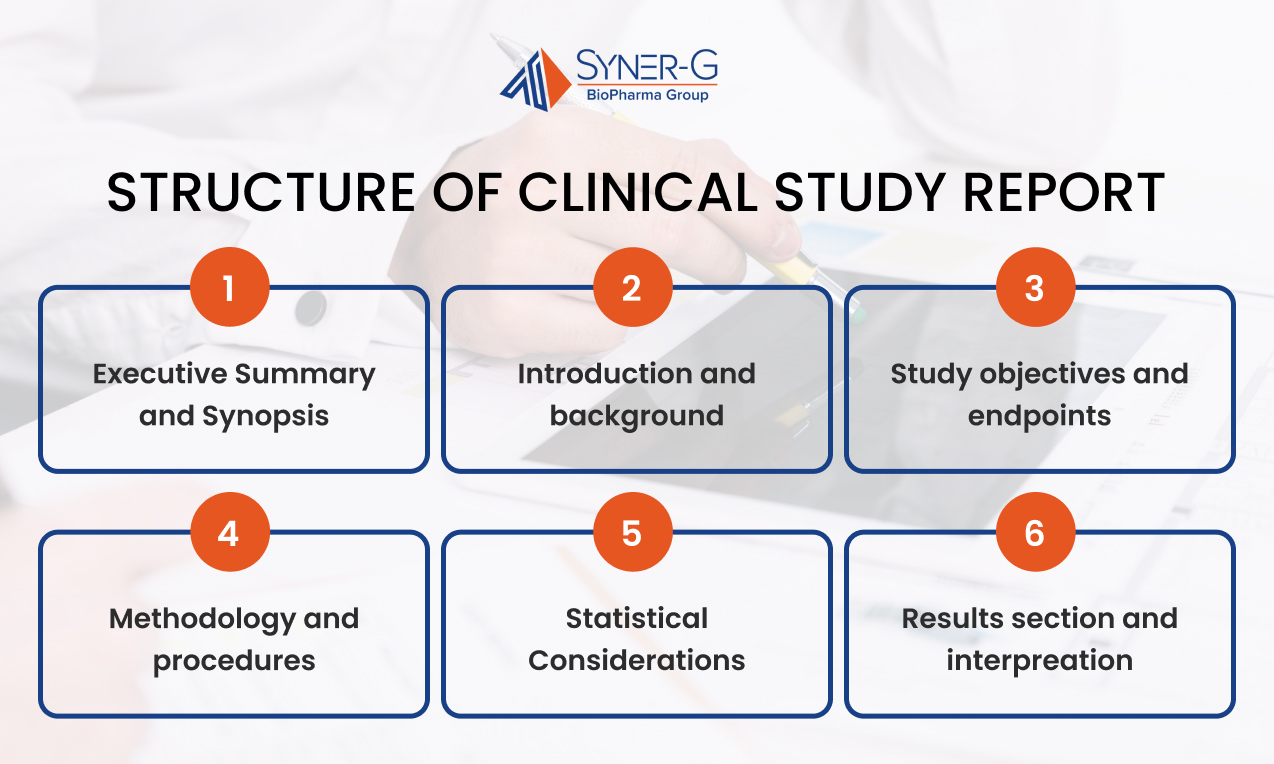
Standard Structure of a CSR
Clinical study reports follow established formatting guidelines developed by international regulatory councils. The structure and content of CSRs are governed by the ICH E3 guideline, which provides internationally harmonized standards for documenting clinical trials in regulatory submissions. This standardized approach facilitates efficient review and ensures consistent information presentation across different studies and sponsors.
The typical structure includes several essential components:
- Executive Summary and Synopsis: Summarizes key findings, methodology, and clinical implications derived from the study data and statistical analysis
- Introduction and Background: Reviews relevant literature and establishes the scientific rationale for conducting the trial within the current therapeutic landscape
- Study Objectives and Endpoints: Documents prespecified endpoints and analysis plans that guide the statistical evaluation and interpretation of results
- Methodology and Procedures: Describes participant selection, randomization procedures, and protocol implementation details required for good clinical practice compliance
- Statistical Considerations: Outlines the statistical analysis plan, sample size calculations, and analytical methods used to evaluate study outcomes
- Results Section: Presents findings systematically, addressing efficacy and safety outcomes with appropriate statistical presentations and confidence intervals
- Safety Assessment: Comprehensive evaluation of adverse events, laboratory abnormalities, and other safety parameters, particularly relevant for life-threatening diseases
- Discussion and Interpretation: Analyzes results within the broader clinical context, acknowledges study limitations, and discusses implications for clinical practice
This framework allows regulatory reviewers to locate specific information efficiently while ensuring comprehensive coverage of all trial aspects.
Who is Responsible for Writing a CSR?
Medical writers typically assume the responsibility of clinical study report development, though the responsibility extends across multiple study team members. These professionals combine regulatory writing expertise with scientific knowledge to produce documents that meet submission requirements. Most medical writers specialize in specific therapeutic areas, allowing them to understand disease-specific regulatory expectations.
Study sponsors maintain oversight throughout the writing process. They ensure that reports support overall development strategies and comply with applicable regulatory guidance. Principal investigators contribute clinical expertise and help interpret results within their therapeutic specialization. Their involvement proves particularly valuable when explaining unexpected findings or addressing methodological questions.
Biostatisticians play an equally important role in report preparation. They generate analytical outputs, verify statistical presentations, and help medical writers interpret complex analytical results. Regulatory affairs professionals review drafts to confirm compliance with current guidelines and submission requirements.
The medical device industry often employs slightly different authorship models compared to pharmaceutical companies. Device studies may involve engineering teams who contribute technical expertise about device performance and safety characteristics. These multidisciplinary teams make sure that reports address both clinical and technical aspects of device evaluation.

How Writers and Statisticians Collaborate
Effective collaboration between medical writers and statisticians begins during protocol development. Writers review the statistical analysis plan to understand planned analyses and identify potential presentation challenges. Early discussions help establish consistent terminology and ensure that statistical concepts will be explained clearly for regulatory audiences.
During the analysis phase, statisticians provide detailed outputs that writers must interpret and contextualize. This process requires ongoing communication for accurate representation of analytical methods and results. Writers often request additional analyses or alternative presentations to support clear narrative development.
Quality control procedures involve multiple review cycles where both professionals verify accuracy and completeness. Statisticians check that statistical presentations remain technically correct while writers make sure that quantitative information integrates logically with clinical discussions. This iterative process continues until both parties confirm that the report accurately reflects the study data.
Regulatory requirements sometimes necessitate specific statistical presentations that may not align with traditional academic reporting conventions. Writers and statisticians must balance regulatory expectations with scientific communication principles, often requiring creative approaches to present complex analyses clearly.
What Drives the Focus of a CSR
Regulatory requirements primarily determine clinical study report content and emphasis. Different regulatory authorities may have varying expectations for the same study, requiring sponsors to adapt their approach accordingly. FDA guidance documents provide specific recommendations for different therapeutic areas and study designs.
The disease indication significantly influences report focus and depth. Studies investigating rare diseases may require different analytical approaches compared to common conditions with established treatment paradigms. Life-threatening diseases demand more comprehensive safety reporting and careful risk-benefit assessment.
Study outcomes also shape narrative emphasis. Positive efficacy results require different presentation strategies compared to studies with negative or inconclusive findings. Failed trials still provide valuable information but require careful interpretation to extract meaningful conclusions for future development decisions.
Market access considerations increasingly influence report development. Health technology assessment bodies require specific types of evidence that may extend beyond traditional regulatory requirements. Study sponsors must anticipate these diverse information needs while maintaining scientific rigor and regulatory compliance.

Where Medical Writers Face the Most Difficulties in CSR Writing
Complex statistical analyses present ongoing challenges for medical writers. Advanced analytical techniques require careful explanation to provide accessibility without oversimplifying critical details. Writers must translate statistical concepts for clinicians and regulators who may have varying levels of statistical expertise.
Data volume and complexity have increased dramatically with modern clinical trials. Electronic data capture systems generate enormous datasets that must be synthesized into coherent narratives. Writers face the challenge of identifying key findings while avoiding information overload that might obscure important messages.
Evolving regulatory expectations create additional difficulties for writers attempting to stay current with guidance documents. International harmonization efforts have improved consistency, but regional differences still exist. Writers must navigate these variations while producing documents that satisfy multiple regulatory authorities.
Timeline pressures frequently complicate the writing process. Regulatory submission deadlines may conflict with optimal writing schedules, forcing writers to balance thoroughness with efficiency. These constraints can compromise document quality if not managed carefully through proper planning and resource allocation.
Methodological flaws or protocol deviations require particularly skillful handling in clinical study reports. Writers must acknowledge limitations honestly while maintaining confidence in study conclusions. This balance requires extensive clinical knowledge and regulatory experience to execute effectively.
The clinical study report remains central to pharmaceutical development and regulatory approval processes. Success requires understanding complex regulatory requirements, maintaining scientific standards, and communicating effectively with diverse stakeholders. As regulations continue evolving, medical writers and their collaborators must adapt while preserving the fundamental principles that ensure reliable clinical evidence generation.

