Navigating the different phases of the regulatory pathway during drug development to achieve FDA approval is a complex and critical process every new drug must undergo. This process, essential for guaranteeing the safety and efficacy of medications, involves a rigorous series of tests and evaluations. At each stage, a thorough evaluation is applied so that only the safest and most effective drugs make it to market.
We’ll break down each phase of the FDA approval process, from preclinical research to post-market surveillance. By understanding these phases, you’ll understand how drugs are tested, evaluated, and ultimately approved for public use.
Preclinical Research
Before a new drug can enter human trials, it undergoes an extensive preclinical research phase. This crucial stage is designed to gather initial data on the drug’s safety and efficacy, setting the foundation for future clinical trials.
Purpose of Preclinical Research
Preclinical research aims to determine whether a drug is safe enough to be tested in humans. This involves evaluating its biological effects, potential toxicity, and overall pharmacological profile. By thoroughly investigating these aspects, researchers can identify any significant risks or adverse effects early in the development process.
Types of Tests Conducted
- Pharmacodynamics: Studies how the drug affects the body, including its mechanisms of action and therapeutic effects.
- Pharmacokinetics: Examines how the body absorbs, distributes, metabolizes, and excretes the drug. Key parameters include absorption rates, bioavailability, half-life, and clearance.
- Toxicology: Assesses the potential toxic effects of the drug, identifying safe dosage ranges and highlighting any harmful side effects. This includes both acute and chronic toxicity studies.
- Genotoxicity: Tests whether the drug can cause genetic mutations or damage to DNA, which could lead to cancer or other serious health issues.
- Carcinogenicity: Long-term studies to determine if the drug has the potential to cause cancer.
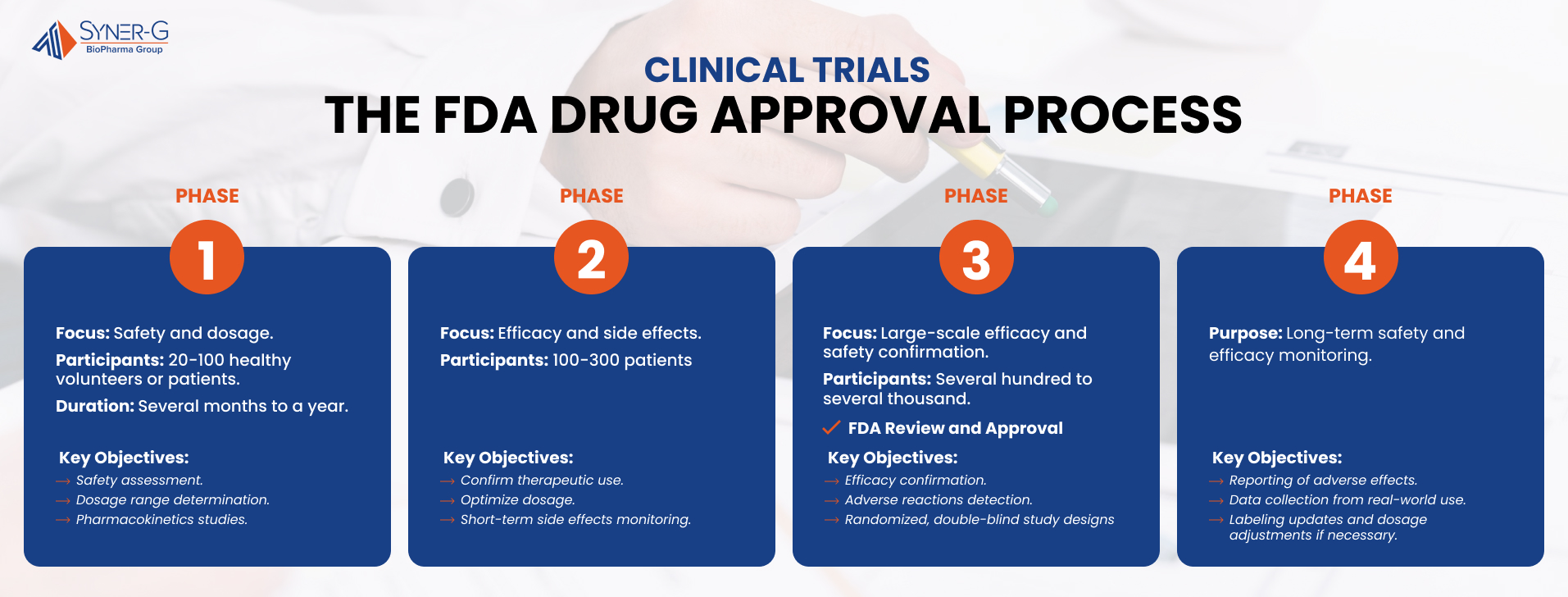
Phase 1 Clinical Trials
After completing preclinical research, a new drug progresses to Phase 1 clinical trials. This initial phase of human testing is critical for understanding how the drug interacts with the human body and determining its safety profile.
Safety and Dosage
Objectives of Phase 1 Trials
The primary objectives of Phase 1 clinical trials are to evaluate the safety of the drug and establish an appropriate dosage range. Researchers aim to identify any potential side effects and determine the optimal dose that balances efficacy with minimal adverse reactions.
Often, Phase 1 trials involve healthy volunteers, which helps isolate the effects of the drug without interference from underlying health conditions. However, in some cases, especially for drugs intended to treat serious or life-threatening conditions, patients with the target condition may be included. This approach can provide early insights into the drug’s therapeutic effects.
The biggest concern in Phase 1 trials is to monitor the safety of the drug. Researchers closely observe participants for any adverse effects and collect data on their severity and frequency. Assessing how well participants tolerate the drug is also crucial, including any discomfort or side effects experienced.
Additionally, pharmacokinetics studies are conducted to understand how the drug is absorbed, distributed, metabolized, and excreted by the body. This helps in determining appropriate dosing intervals and understanding the drug’s behavior within the human system.
Typical Duration and Sample Size
Phase 1 trials typically last several months to a year, depending on the nature of the drug and the speed of participant recruitment. These trials usually involve a small group of 20 to 100 participants. The limited size allows for close monitoring and detailed data collection without exposing too many individuals to potential risks.
Phase 1 clinical trials are a pivotal step in drug development, laying the groundwork for subsequent phases by providing essential safety and dosage information.
Phase 2 Clinical Trials
After establishing the initial safety and dosage parameters in Phase 1, a drug moves into Phase 2 clinical trials. This phase builds upon the previous findings, aiming to further assess the drug’s efficacy and monitor for any side effects in a larger group of participants. A major component of this phase is honing in on the therapeutic dose. Typically, it is also the first time the medicine is sent home with participants to self-administer, allowing them to report adverse events (AEs) in a real-world setting.
Efficacy and Side Effects
Researchers aim to confirm that the drug works as intended for its specific therapeutic use and to identify any short-term side effects that may not have been apparent in Phase 1.
Phase 2 trials involve a larger group of participants compared to Phase 1, typically ranging from 100 to 300 individuals. These participants are often patients who have the condition the drug is intended to treat, providing a more accurate assessment of the drug’s effectiveness and side effects in the target population.
During Phase 2 trials, researchers focus on determining the optimal dose that maximizes efficacy while minimizing side effects. This involves testing various dosages to find the best balance. Monitoring short-term side effects is crucial in this phase, as it helps refine the drug’s safety profile and dosage recommendations for future trials.
Data collection in Phase 2 trials is comprehensive and involves various methods to ensure accuracy and reliability. Clinical endpoints are established to measure the drug’s efficacy, such as improvement in symptoms or biomarkers specific to the condition being treated. Researchers also gather data on adverse effects, recording the type, frequency, and severity of any side effects experienced by participants. Statistical analysis is then used to evaluate the data, providing a detailed understanding of the drug’s performance and safety.
Phase 3 Clinical Trials
Phase 3 clinical trials represent a critical juncture in the drug development process, where the primary goal is to confirm the drug’s effectiveness and safety on a larger scale. This phase provides the comprehensive data needed for regulatory approval.
Confirmation and Monitoring
This phase aims to confirm the findings from earlier trials and to detect any less common adverse reactions that may not have appeared in smaller groups.
Phase 3 trials involve large-scale testing, typically including several hundred to several thousand participants. This diverse participant pool ensures that the data reflects a broad range of demographics, enhancing the generalizability of the trial results. Including various ages, genders, ethnicities, and comorbid conditions helps to understand how the drug performs across different segments of the population.
Researchers document both the efficacy of the drug and any adverse reactions. This involves detailed record-keeping of the drug’s effects on the target condition, improvements in the patient’s health, and any side effects experienced.
To ensure comprehensive evaluation, Phase 3 trials build on the data from previous phases by testing the drug in larger populations and diverse clinical settings. These trials often use randomized and double-blind study designs, which are common in all phases, to eliminate bias and guarantee reliable results. In a randomized trial, participants are randomly assigned to receive either the drug under investigation or a placebo/control treatment. The primary goal in Phase 3 is to confirm the drug’s effectiveness, monitor side effects, and collect information that will allow the drug to be used safely.
In a double-blind study, neither the participants nor the researchers know who is receiving the active drug versus the placebo, which helps prevent bias in reporting and assessing outcomes.
Upon completing Phase 3 trials, the collected data is prepared for submission to the FDA in the form of a New Drug Application (NDA). This submission marks the beginning of the regulatory review process, where the FDA will evaluate the drug’s safety and efficacy data to determine whether it can be approved for public use.
FDA Review and Approval
The NDA is a comprehensive document that includes all the data and analyses from the preclinical and clinical trials. Regulatory affairs professionals help create this document for submission. Key components of the NDA include:
- Clinical Data: Detailed results from all phases of clinical trials, demonstrating the drug’s safety and efficacy.
- Non-Clinical Data: Results from preclinical studies, including animal testing.
- CMC Information: Details on the drug’s production, including methods and quality control measures.
- Labeling: Proposed labels and information for healthcare providers and patients, explaining the drug’s use, dosage, and potential side effects.
- Risk Management: Plans for monitoring the drug’s safety post-approval.
The FDA review process for medications typically takes 10 months for standard review or 6 months for priority review. The review involves a thorough evaluation by a team of experts in various fields, including pharmacology, toxicology, and clinical medicine. This team assesses the submitted data to determine whether the drug meets the necessary standards for safety and efficacy.
At the end of the review process, the FDA can decide to:
- Approve the Drug: The drug is deemed safe and effective for its intended use, allowing it to be marketed and prescribed.
- Reject the Drug: The drug does not meet the required standards, and the application is denied.
- Request Additional Information: The FDA may ask for more data or further studies before making a final decision.
Related Article: How Long Does FDA Approval Take After Phase 3
Phase 4 Clinical Trials
After a drug receives FDA approval and enters the market, the journey doesn’t end there. Phase 4 clinical trials, also known as post-market surveillance, play a crucial role in monitoring the long-term effects and ensuring the continued safety and efficacy of the drug.
Post-Market Surveillance
The importance of ongoing monitoring in Phase 4 cannot be overstated. Even after rigorous testing in earlier phases, some side effects or risks may only become apparent when the drug is used by a larger and more diverse population over a longer period. Ongoing surveillance helps detect these issues early, making sure that any necessary actions can be taken to protect public health.
In Phase 4 trials, healthcare providers and patients are encouraged to report any adverse effects experienced while using the drug. This real-world data is important for assessing the long-term safety profile of the medication. Data collection and analysis help identify rare or delayed side effects that were not evident in earlier trials.
The findings from post-market surveillance can significantly impact the labeling and usage recommendations of the drug. If new risks are identified, the FDA may require updates to the drug’s labeling to inform healthcare providers and patients of these risks. Additionally, dosage recommendations may be adjusted based on long-term efficacy and safety data. In some cases, new warnings or contraindications might be added to ensure safe use.
From Discovery to Prescription: The Path of Drug Approval
Each phase of the FDA approval process ensures that only the safest and most effective medications reach the public. Drug development consultants can create a smooth process for drug approval, making sure it meets regulatory standards with a well-crafted strategy.
This process safeguards public health, providing confidence in the treatments we rely on every day.

