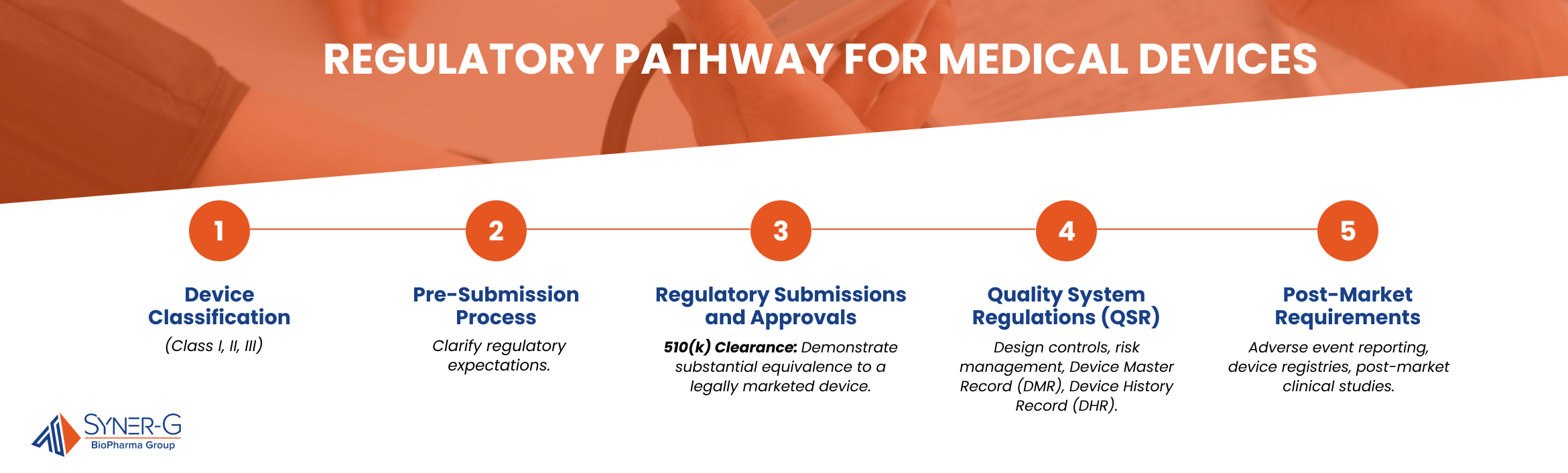
The complete regulatory pathway for medical devices from concept to market is filled with intricate steps, evaluations, and planning. It’s an essential path for bringing safe and effective medical devices to the public. This process, while complex, is designed to guarantee that every device meets stringent safety and efficacy standards.
Understanding the initial steps in the regulatory pathway is crucial for setting a strong foundation for your medical device’s approval process. This stage involves comprehending device classification and engaging in the pre-submission process to pave the way for a smooth journey.

Device Classification
Understanding the classification of your medical device is the first step in the regulatory pathway. Device classification determines the level of regulatory control necessary to guarantee the safety and efficacy of the device. It’s a process that helps to identify the level of risk associated with a medical device.
This classification guides the regulatory requirements that must be met for the device to gain market approval. Proper classification is essential as it dictates the pre-market submission requirements, necessary controls, and regulatory oversight.
Types of Device Classifications (Class I, II, III)
Medical devices are classified into three categories. Class I devices present minimal potential risk to users and are often simpler in design, such as bandages and handheld surgical instruments. Most Class I devices are exempt from premarket notification.
Class II devices pose a moderate risk and require more stringent regulatory controls, such as powered wheelchairs and infusion pumps. These typically require premarket notification through the 510(k) process.
Class III devices sustain or support life, are implanted, or present a potential high risk of illness or injury, like pacemakers and stents. These require premarket approval (PMA) demonstrating safety and efficacy through extensive clinical data.
Several factors influence the classification of a medical device, including its intended use, the potential risk to patients, the technology used, and whether the device is life-sustaining or life-supporting. The classification process considers these elements to apply the appropriate level of regulatory scrutiny.
Premarket Notification (510(k)) vs. Premarket Approval (PMA)
Premarket Notification (510(k)):
- A regulatory process where manufacturers must demonstrate that their medical device is substantially equivalent to an already legally marketed device.
- Typically required for Class I and II devices.
- Faster and less costly than PMA, usually taking a few months for FDA clearance.
Premarket Approval (PMA):
- A more rigorous process required for Class III devices, which pose the highest risk.
- Involves providing extensive scientific evidence proving the device’s safety and effectiveness.
- Lengthy and expensive, often taking several months to years for FDA approval.

Pre-Submission Process
Engaging in the pre-submission process is a proactive step that can significantly impact the success of a medical device’s regulatory journey.
Purpose of the Pre-Submission Process
The pre-submission process allows device sponsors to obtain feedback from the FDA before submitting a formal application. This early interaction helps clarify regulatory expectations, refine study designs, and address potential issues upfront. By doing so, it could streamline the subsequent review process and increase the likelihood of a successful submission.
A pre-submission package typically includes a comprehensive description of the device, its intended use, and a summary of the proposed testing and clinical study plans. It should also detail any specific questions or areas where FDA input is sought. The package serves as a basis for discussion during pre-submission meetings with the FDA.
Early engagement with the FDA provides several benefits. First, early feedback helps clarify the necessary regulatory requirements and expectations, reducing the risk of unexpected hurdles during the formal review process.
Second, the FDA can provide valuable input on study design and data requirements, enhancing the quality and relevance of the submitted data. Lastly, addressing potential issues early in the development process helps mitigate risks and prevents costly delays or rejections later on.

Regulatory Submissions and Approvals
This stage involves several key processes, including 510(k) clearance, premarket approval (PMA), and the De Novo classification pathway.
510(k) Clearance
The 510(k) clearance is a premarket submission to the FDA demonstrating that a device is at least as safe and effective, or substantially equivalent, to a legally marketed device not subject to PMA. Its main purpose is to simplify the approval process for new devices that do not pose new risks by leveraging existing approved devices.
To get 510(k) clearance, the new device must have the same intended use and technological characteristics as a predicate device. If there are different technological characteristics, it must be shown that these differences do not raise new safety and effectiveness concerns.
The 510(k) submission process involves comparing the new device with the existing device, compiling a submission package with detailed descriptions, labeling, and performance data, and submitting it to the FDA. The FDA reviews the submission and, if satisfied, grants clearance, allowing the device to be marketed.
Premarket Approval (PMA)
Premarket Approval (PMA) is the FDA’s rigorous scientific and regulatory review to evaluate the safety and effectiveness of Class III medical devices, which are those that sustain or support life, are implanted, or pose a high risk of illness or injury.
Criteria for PMA Submission
PMA is required for Class III devices and involves extensive preclinical and clinical data to demonstrate that the device provides reasonable assurance of safety and effectiveness. This includes results from well-controlled clinical trials.
The PMA process begins with preclinical testing and clinical trials conducted under an Investigational Device Exemption (IDE). The PMA application includes all data, manufacturing information, labeling, and instructions for use. The FDA’s review includes detailed analysis and advisory panel meetings, and the process can take several months to years.
De Novo Classification
The De Novo classification pathway is for novel medical devices that present low to moderate risk and do not have a predicate device. It is an alternative to the 510(k) pathway for devices that cannot be cleared through substantial equivalence but do not require the rigorous PMA process.
Criteria for De Novo Submission
Devices must be new and not substantially equivalent to any existing legally marketed device but must demonstrate reasonable assurance of safety and effectiveness for their intended use. They should not pose significant risks requiring PMA.
The De Novo process involves submitting a petition to the FDA with detailed information about the device, its intended use, and supporting evidence of safety and effectiveness. The FDA reviews the petition, and if the device is deemed low to moderate risk with adequate controls, it grants De Novo classification, allowing the device to be marketed.

Quality System Regulations (QSR)
Adhering to Quality System Regulations (QSR) is crucial in the manufacturing of medical devices. These regulations ensure devices meet the necessary standards for safety and effectiveness throughout their lifecycle.
Establishing a Quality Management System (QMS)
While a Quality Management System (QMS) for medical devices shares some similarities with that for regular drugs, it includes unique components tailored specifically to medical devices. Key differences include rigorous design controls, comprehensive risk management, and detailed documentation requirements such as the Device Master Record (DMR) and Device History Record (DHR). Additionally, robust procedures for Corrective and Preventive Action (CAPA), specific labeling and packaging controls, thorough complaint handling, and extensive post-market surveillance are integral to the QMS for medical devices. These elements ensure that devices are safe, effective, and meet stringent regulatory requirements.
Compliance with FDA’s Quality System Regulation (QSR)
Compliance with the FDA’s QSR is mandatory for medical device manufacturers. The QSR outlines specific requirements for a QMS that emphasize the need for robust design controls, production processes, and quality assurance mechanisms unique to medical devices. Understanding these distinct requirements is essential, and consulting with experts can help manufacturers navigate these complexities. Adhering to these regulations helps produce devices that consistently meet safety and performance standards, reducing the risk of defects and recalls.
Good Manufacturing Practices (GMP)
Good Manufacturing Practices are a set of guidelines that govern the production and quality control of medical devices. These practices ensure that products are consistently produced and controlled according to quality standards, minimizing risks associated with manufacturing defects.
Implementation of GMP in Device Manufacturing
Implementing GMP in device manufacturing involves several critical steps:
- Facility Design and Maintenance: Ensuring that manufacturing facilities are designed and maintained to prevent contamination and allow for efficient cleaning and maintenance.
- Process Validation: Validating manufacturing processes to ensure they produce consistent, high-quality products.
- Personnel Training: Providing comprehensive training for all personnel involved in the manufacturing process, ensuring they understand and adhere to GMP requirements.
- Quality Control: Establishing procedures for inspecting and testing raw materials, intermediate products, and finished devices to ensure they meet specifications.
Continuous Compliance and Audits
Maintaining continuous compliance with GMP requires ongoing effort and vigilance. Regular internal and external audits are conducted to verify that all aspects of the manufacturing process adhere to GMP standards.
These audits help identify areas for improvement and ensure that any deviations are promptly addressed. Continuous compliance not only meets regulatory requirements but also enhances product quality and reliability, fostering trust among healthcare providers and patients.
Post-Market Requirements
After a medical device enters the market, ongoing monitoring is essential to maintain its safety and effectiveness.

Post-Market Surveillance
Post-market surveillance identifies any adverse events or new risks that arise during widespread use.
Methods of Post-Market Surveillance
Adverse event reporting, device registries, and post-market clinical studies are key methods for gathering real-world performance data.
The FDA oversees post-market activities, reviewing adverse event reports, conducting inspections, and evaluating data to ensure continued device safety. Regulatory actions may be taken if significant safety concerns arise.
Recalls and Corrections
Recalls are initiated when a device is found to be defective or harmful, violates regulations, or poses new significant risks.
The recall process includes notifying the FDA and affected parties, developing a recall strategy, executing the recall, and monitoring its effectiveness.
Reporting Requirements and Corrective Actions
Manufacturers must report recalls to the FDA and provide updates. Corrective actions, such as design changes or process improvements, are implemented to prevent recurrence.
Post-market requirements, including surveillance and recall procedures, are vital for maintaining the safety and effectiveness of medical devices, protecting patients, and ensuring continued regulatory compliance.
Making Medical Devices Market Ready
By understanding and adhering to the regulations that ensure the safety of a medical device, manufacturers can confidently navigate the complex approval process. With a thorough grasp of these processes, manufacturers can successfully bring innovative and reliable medical devices to market.

